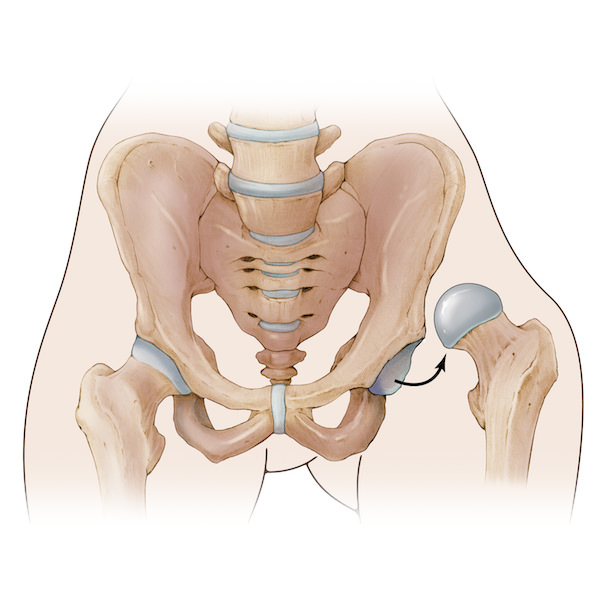
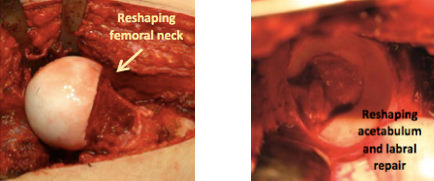
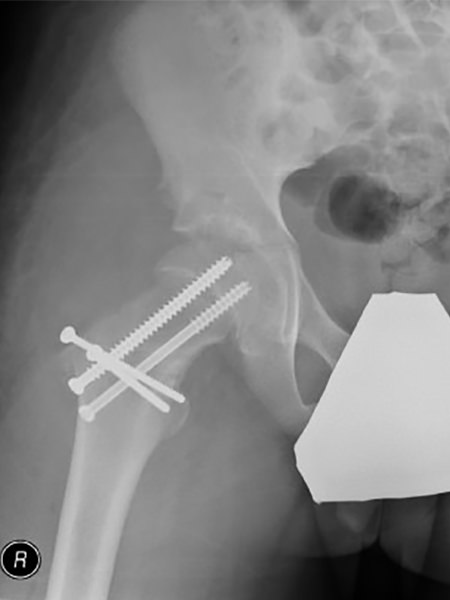
The surgical hip dislocation approach is a combination of the posterior-lateral approach with a trochanteric flip and anterior dislocation of the hip. The advantage of this technique is access to the entire hip joint without compromising the blood supply to the femoral head.
Indications / Candidacy
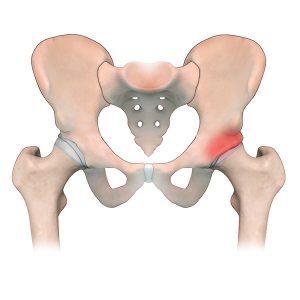
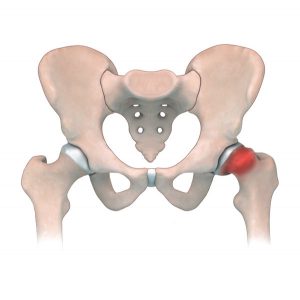
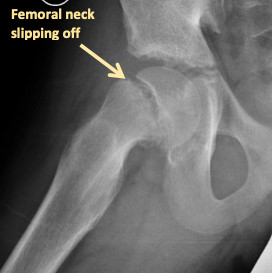
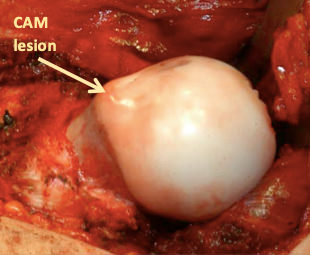
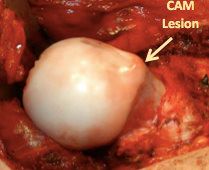
Surgical hip dislocation can be used to correct a slipped deformity of the femoral head, or impingement of the femoral neck or acetabulum that can be found in both SCFE and Femoral-acetabular impingement. Both of these conditions can cause pain and damage to the hip joint that affects a patient’s ability to comfortably perform activities.
Good candidates for this surgery may have:
- Previous trauma to the hip leading to deformities of the head and neck of the femur
- SCFE (slipped capital femoral epiphysis)
- Femoral-acetabular impingement (FAI) and labral tears
- Pain related to poor hip biomechanics that worsens with activity
- Painful and decreased range of motion related to hip deformities


Treated Conditions
The Canadian Limb Lengthening Center offers a team of experienced surgeons, nurses and physiotherapists that make patients feel supported throughout their entire treatment process. Our ability to treat complex orthopedic conditions with a holistic approach gives our patients the best possible outcomes. We pride ourselves in providing highly specialized, expert care that helps patients and families dealing with Perthes disease, among many other diseases. To learn more about conditions treated using surgical hip dislocation, follow the links below:
Surgical Technique
Results
Surgical hip dislocation improves lower limb length discrepancy, gait, and range of motion at the hip for patients. The result from surgery can improve hip biomechanics and function. Our patients see improvements in quality of life after surgery and experience less complications, pain and discomfort later in life. This approach allows for repair of intra-articular structures and may help prevent osteoarthritis from progressing in future.


Potential Complications
As with any surgical procedure, the Surgical hip dislocation technique can have difficulties and complications. In most cases, our team of specialist can address these concerns without compromising the end results or outcome. Complications and side effects may include:
- Avascular necrosis (AVN) of the femoral head
- Nerve injury to the sciatic nerve (Neuropraxia)
- Trochanteric non-union or malunion
- Heterotopic ossification
- Infection of the bone (osteomyelitis)
- Progression of arthritis
- Neurovascular injury (rare)
- Deep vein thrombosis (rare)
AM I A CANDIDATE?
Are you experiencing an orthopedic condition and would like to improve your physical capabilities?
Or you simply would like to achieve your long-lasting dream of improving your height?
Let us help you achieve your optimal health and wellness in a professional setting.
Let’s open up a discussion to help you achieve your goals.




Highly specialized expert care at CLLC
At the Canadian Limb Lengthening Centre we offer complex deformity correction and limb lengthening surgeries performed by experienced surgeons with the most up to date technologies. When it comes to your care, and treatment of deformity and limb length discrepancy, our surgeons have extensive training and experience.