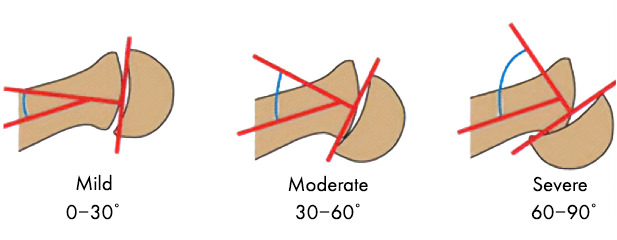
SCFE is a condition that affects the femoral head at the level of the growth plate where the femoral head slips off the neck. In lay terms, can be described as the ice cream falling off the ice-cream cone. Treatment with In Situ Pinning for SCFE varies depending on the type of slip and severity. The severity is usually described as mild (0-30 degrees), moderate (30-60) or severe (over 60 degrees) slip. In situ fixation is only recommended for mild to moderate slips. In some cases, our team might also recommend pinning the contralateral hip (other side).
Indications / Candidacy
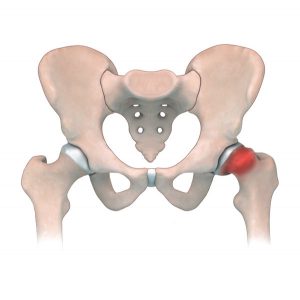
Patients with SCFE typically present with hip (groin) or knee pain often associated with a limp. Parents may notice that the affected leg is slightly rotated externally with walking. This condition can be diagnosis with radiographs of the hip. SCFE most often happens in overweight adolescents between the ages of 10-16.
Good candidates for in situ pinning surgery have:
- Stable, mild to moderate SCFE (Slipped Capital Femoral Epiphysis)
- Femoral neck fractures or risk of fracture in patients with skeletal immaturity



Treated Conditions
The Canadian Limb Lengthening Center offers a team of experienced surgeons, nurses and physiotherapists that make patients feel supported throughout their entire treatment process. Our ability to treat complex orthopedic conditions with a holistic approach gives our patients the best possible outcomes. We pride ourselves in providing highly specialized, expert care. To learn more about SCFE, a condition commonly treated using in situ pinning techniques, follow the link below:
Surgical Technique
1 Fixation In-situ – closing the growth plate
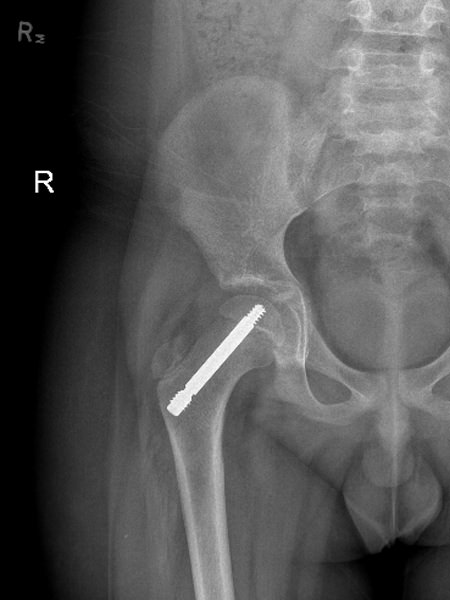
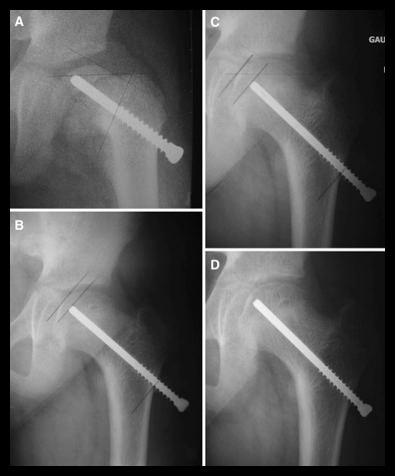
Fixation In-situ is the classic treatment for a SCFE (especially mild to moderate), where the femoral head is kept from further slipping off the neck by 1 or 2 large screws that eventually cause the growth plate to close. The in situ screw is fixated in a center-center position, perpendicular to the physis (growth plate) in order to stabilize it without any forceful reduction.
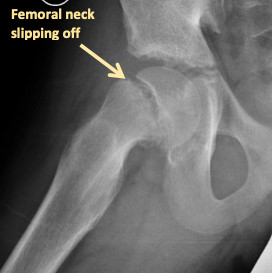
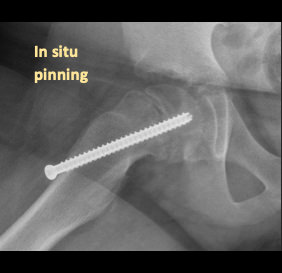
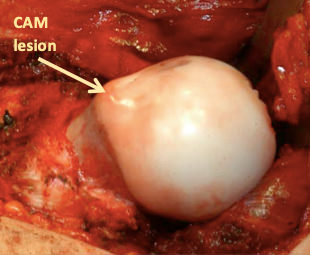
Closing the growth plate was classically believed to be the safest way to prevent the slip from further progressing (gold standard). The problem with this treatment is that does not correct the underlying slip deformity, which can lead to femoral-acetabular impingement (FAI) causing labral tears and pre-mature wearing of the hip (Figure 3). Furthermore, closing the growth plate on only one side can lead to an eventual difference in the leg lengths for the patient.
2 Surgical Approach for In-Situ pinning:
- Patient is placed on a radiolucent table
- The leg is placed with the knee cap (patella) pointing towards the ceiling. There are no attempts to reduce the position of the slip with any excessive rotation.
- A guide wire is placed in the hip, in the center-center position under radiographic guidance to be perpendicular to the physis.
- A skin incision is made on the guide wire, the length is measured and a cannulated drill is used over the guide-wire.
- The screw of the correct length is then positioned.
- Final radiographs are taken intra-operatively to ensure that the screw is not protruding into the hip joint and that its position is center-center
- The skin is closed.

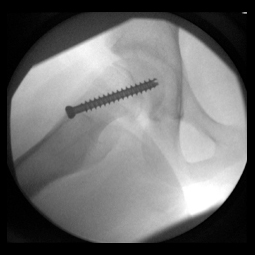
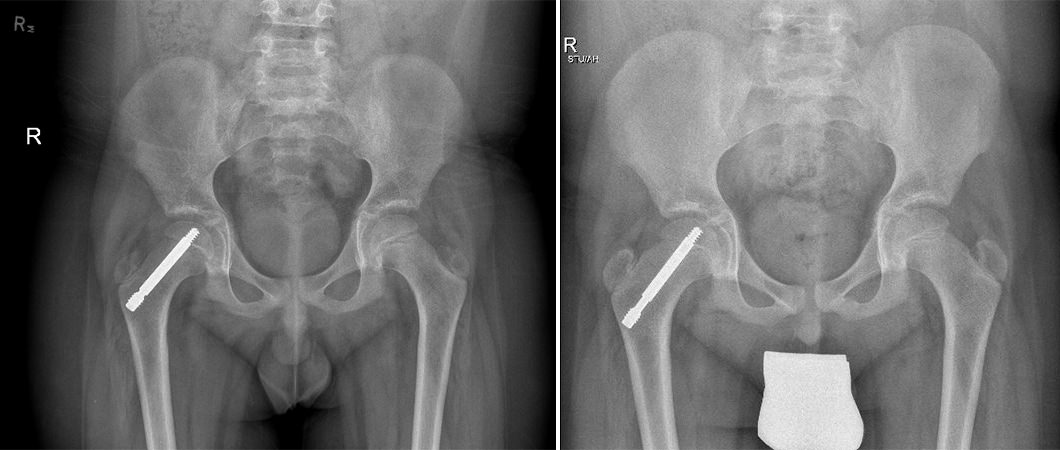
3 Leaving the growth plate open (AKA Non-fusion technique)
An alternative approach to treating slips is to stabilize the physis while leaving the growth plate open. This treatment allows the deformity to remodel and prevents any limb length discrepancies from occurring.
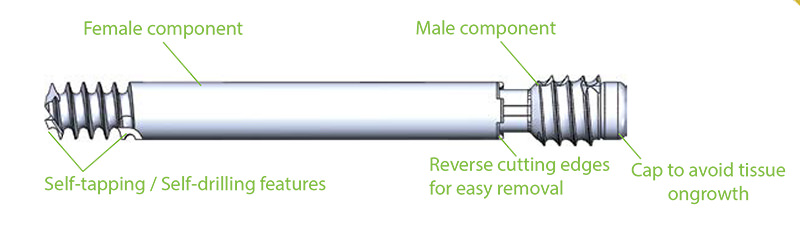
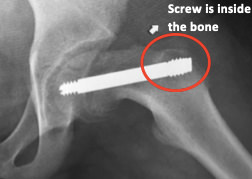
See in imagery an example of a laterally threaded screw that is placed through the femoral neck and attaching it to the femoral head. It prevents further slippage while allowing the neck to continue to grow (i.e. leaving the growth plate open) and allows for the deformity (bump) to remodel during the growth process. However, the pin is left outside of the bone laterally (proud) in order to allow for growth which can be hindering for certain patients. Other similar screws are medially threaded screws, Hanssen pin and smooth pins. All of these types of pins and screws involve either leaving the screw proud or having to return to the OR in order to extract them and replace them with longer ones during growth.
THE FREE GLIDING TELESCOPIC SCREW
The Free gliding telescopic screw follows the same principle of stabilizing the physis (growth plate) while allowing continued growth. The FG screw was co-invented by the founder of our Center, Dr. Marie Gdalevitch herself, and is composed of two parts, a male and a female component that are reversed to allow for telescopic growth and stability of the physis. This screw avoids protruding screw placement as it is placed fully within the bony structures. It stabilizes the slip and allows for bump remodeling if sufficient growth remains. This is our preferred hardware of choice for in situ pinning and we firmly believe that non-fusion techniques have many advantages over traditional in situ fusion for the treatment of SCFE.
The technique is very similar to the in situ pinning technique.



Results
Early detection and proper treatment of SCFE can lead to very functional and comfortable outcomes for our patients. With treatment we can avoid more serious complications such as rapid degeneration of the femoral head and/or painful arthritis in the hip joint. After treatment patients have improved gait and range of motion as well as decreased pain. Our patients see improvements in quality of life after surgery and experience less complications later in life.
Potential Complications
As with any surgical procedure, In Situ Pinning for SCFE can have difficulties and complications. In most cases, our team of specialists can address these concerns without compromising the end results or outcome. Complications and side effects may include:
- Osteonecrosis
- Osteoarthritis
- Chondrolysis
- Progressive decline of hip function (mobility, strength)
- Joint space narrowing
- Nerve injury (Neuropraxia)
- Infection of bone or joint
AM I A CANDIDATE?
Are you experiencing an orthopedic condition and would like to improve your physical capabilities?
Or you simply would like to achieve your long-lasting dream of improving your height?
Let us help you achieve your optimal health and wellness in a professional setting.
Let’s open up a discussion to help you achieve your goals.




Highly specialized expert care at CLLC
At the Canadian Limb Lengthening Centre we offer complex deformity correction and limb lengthening surgeries performed by experienced surgeons with the most up to date technologies. When it comes to your care, and treatment of deformity and limb length discrepancy, our surgeons have extensive training and experience.